Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (21): 3423-3429.doi: 10.3969/j.issn.2095-4344.2704
Previous Articles Next Articles
Systematic evaluation and meta-analysis of total hip arthroplasty with three-dimensional printing model in preoperative planning
Yan Yan1, Zhao Yan1, Fu Fanyu2, He Haijun1
- 1Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China; 2Guizhou University of Traditional Chinese Medicine, Guiyang 550002, Guizhou Province, China
-
Received:2019-12-09Revised:2019-12-12Accepted:2020-01-16Online:2020-07-28Published:2020-04-19 -
Contact:He Haijun, Master, Chief physician, Master’s supervisor, Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China -
About author:Yan Yan, Master candidate, Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China -
Supported by:the National Natural Science Foundation of China, No. 81873322
CLC Number:
Cite this article
Yan Yan, Zhao Yan, Fu Fanyu, He Haijun. Systematic evaluation and meta-analysis of total hip arthroplasty with three-dimensional printing model in preoperative planning[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(21): 3423-3429.
share this article
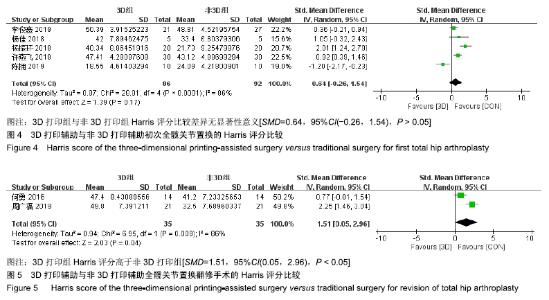
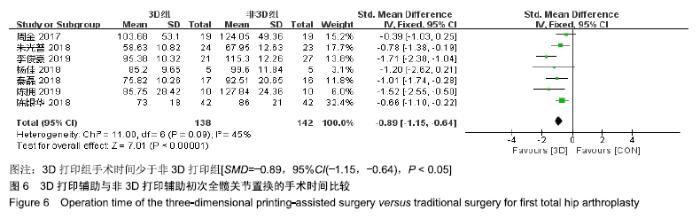
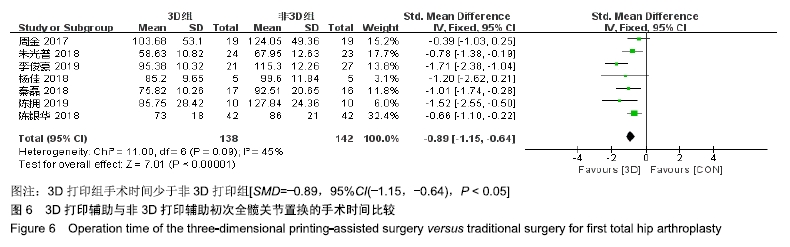
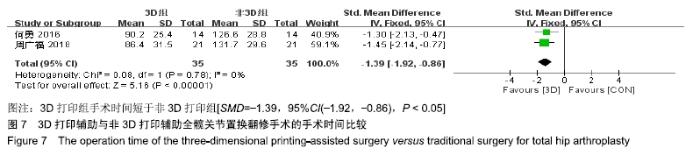
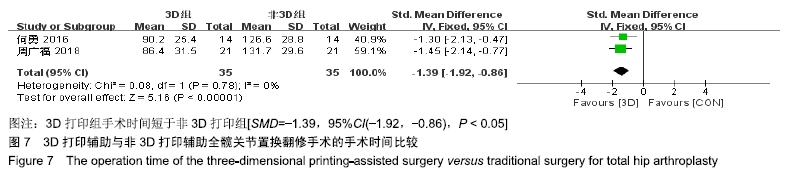
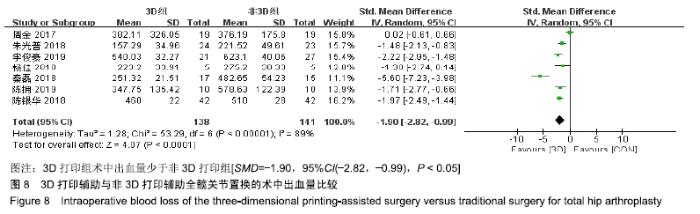
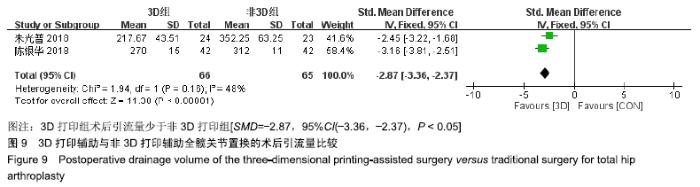
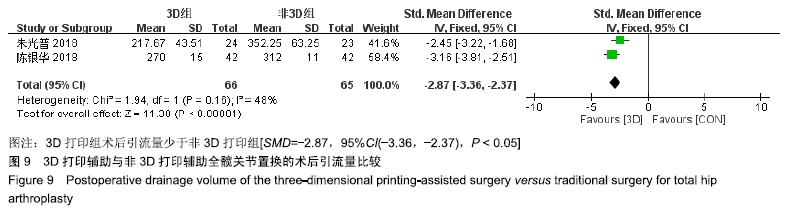
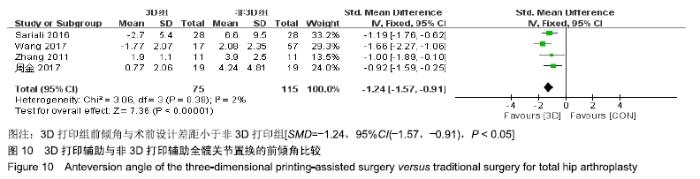
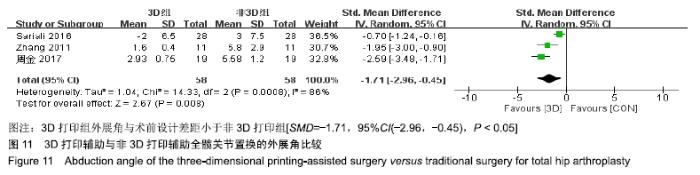
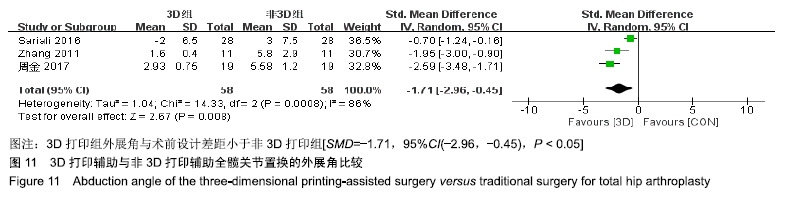
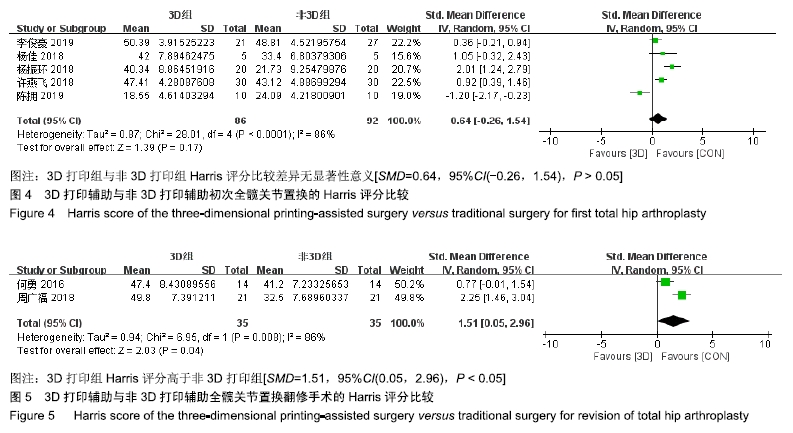
2.3 Harris评分 14篇文献中有8篇文献研究了Harris评分,其中初次全髋关节置换手术有6篇,全髋关节置换翻修手术2篇,但其中1篇未提及标准差,故不纳入分析。 2.3.1 初次全髋关节置换手术Harris评分比较 此次Meta分析纳入5个研究[15-16,20-22],共178例患者,其中3D打印组86例,非3D打印组92例。各研究间存在统计异质性(P < 0.000 01,I2=86%),故选用随机效应模型合并结果。Meta分析结果显示,两组Harris评分比较差异无显著性意义[SMD=0.64,95%CI(-0.26,1.54),P > 0.05],见图4。 与传统人工髋关节置换手术相比,3D打印辅助人工髋关节置换手术的Harris评分无明显差别。 2.3.2 翻修手术Harris评分比较 此次Meta分析纳入2个研究[23,25],共70例患者,其中3D打印组35例,非3D打印组35例。各研究组间存在统计异质性(P < 0.1,I2=86%),故选用随机效应模型合并结果。Meta分析结果显示,3D打印组Harris评分高于非3D打印组[SMD=1.51,95%CI (0.05,2.96),P < 0.05],见图5。 "
| [1] FERGUSON RJ, PALMER AJ, TAYLOR A, et al. Hip replacement. Lancet.2018;392(10158):1662-1671. [2] 郑志博,冯宾,董玉雷,等.全髋关节置换术后脱位因素分析及防治策略[J].中华骨与关节外科杂志,2016,9(3):198-203. [3] UGBEYE ME, LAWAL WO, AYODABO OJ, et al. An Evaluation of Intra- and Post-operative Blood Loss in Total Hip Arthroplasty at the National Orthopaedic Hospital, Lagos.Niger J Surg.2017;23(1):42-46. [4] MACDONALD E, WICKER R. Multiprocess 3D printing for increasing component functionality.Science. 2016;353(6307):aaf2093. [5] 马晨光,纪颖,薛迪.3D打印技术骨科临床应用效应系统性综述[J].中国医院管理,2017,37(5):35-38. [6] 鲍立杰,张志平,吴培斌.3D打印技术在骨科的研究及应用进展[J].中国矫形外科杂志,2015,23(4):325-327. [7] 卢鹏,田文.3D打印技术在骨科及手外科领域的应用研究进展[J].中国骨与关节杂志,2017,6(5):348-351. [8] LIAW CY, GUVENDIREN M. Current and emerging applications of 3D printing in medicine.Biofabrication. 2017;9(2):024102. [9] LUO Q, LAU T, FANG C, et al. Application of three-dimensional printing technique in orthopaedics. Chin J Reparative Reconstructive Surg. 2014;28(3):268. [10] VAISH A, VAISH R. 3D printing and its applications in Orthopedics.J Clin Orthop Trauma. 2018;9(Suppl 1):S74-S75. [11] BAGARIA V,BHANSALI R,PAWAR P.3D printing- creating a blueprint for the future of orthopedics: Current concept review and the road ahead!J Clin Orthop Trauma.2018;9(3):207-212. [12] GANGULI A, PAGAN-DIAZ GJ, GRANT L, et al. 3D printing for preoperative planning and surgical training: a review.Biomed Microdevices. 2018;20(3):65. [13] FANG C, CAI H, KUONG E, et al. Surgical applications of three-dimensional printing in the pelvis and acetabulum: from models and tools to implants. Chirurgische Anwendungen des 3 dimensionalen Drucks an Becken und Acetabulum: von Modellen und Instrumenten zu Implantaten.Unfallchirurg. 2019;122(4):278-285. [14] 黄幼怡,袁伟.3D打印技术与髋关节疾病的治疗[J].中国组织工程研究, 2019,23(34):5538-5543. [15] 陈拥,张斌.3D打印技术辅助全髋关节置换治疗成人发育性髋关节发育不良[J].中国组织工程研究,2019,23(36):5772-5776. [16] 李俊豪,张帅,黄其志,等.应用数字化设计结合3D打印技术人工全髋关节置换手术治疗先天性髋关节发育不良的临床研究[J].中国医学创新,2019, 16(8):1-5. [17] 陈银华,孙天祥,钟易林.3D打印技术制造骨盆模型对DDH患者进行人工髋关节置换术的研究[J].山西医科大学学报,2018,49(2):178-181. [18] 朱光普.3D打印在全髋关节置换术治疗成人发育性髋关节发育不良患者中的应用[J].医药论坛杂志,2018,39(3):49-51,54. [19] 秦磊,李洪彪,韩修福,等.3D打印技术在成人先天性髋关节发育不良Crowe Ⅳ型人工全髋关节置换术应用分析[J].世界最新医学信息文摘, 2018,18(67):68,71. [20] 许燕飞,郭英,艾元亮, 等.3D打印辅助术前设计指导成人髋发育不良全髋置换术与传统术前设计近期疗效分析比较[J].医药前沿,2018,8(16): 156-157. [21] 杨佳,杨毅,赵云宏,等.应用3D打印技术联合组配式S-ROM假体人工髋关节置换术治疗成人Crowe Ⅳ DDH[J].昆明医科大学学报,2018,39(5): 83-89. [22] 杨振环,王晖,葛志强,等.骨小梁3D打印在人工髋关节的应用[J].川北医学院学报,2018,33(1):4-6,10. [23] 周广福,朱伟民,唐本森,等.3D打印技术在髋关节置换术后感染Ⅱ期翻修手术中应用[J].重庆医学,2018,47(13):1746-1748. [24] 周金,刘炯,杨砥,等.3D打印技术辅助成人DDH初次THA的髋臼置入[J].中国矫形外科杂志,2017,25(23):2182-2186. [25] 何勇,刘欣伟,张敬东,等.3D打印技术在髋关节置换术后感染Ⅱ期翻修手术中应用[J].临床军医杂志, 2016,44(10):999-1002,1005. [26] WANG S, WANG L, LIU Y, et al. 3D printing technology used in severe hip deformity.Exp Ther Med. 2017;14(3):2595-2599. [27] SARIALI E, BOUKHELIFA N, CATONNE Y, et al. Comparison of Three-Dimensional Planning-Assisted and Conventional Acetabular Cup Positioning in Total Hip Arthroplasty: A Randomized Controlled Trial.J Bone Joint Surg Am. 2016;98(2):108-116. [28] ZHANG YZ, CHEN B, LU S, et al. Preliminary application of computer-assisted patient-specific acetabular navigational template for total hip arthroplasty in adult single development dysplasia of the hip. Int J Med Robot.2011;7:469-474. [29] HUGHES AJ, DEBUITLEIR C, SODEN P, et al. 3D Printing Aids Acetabular Reconstruction in Complex Revision Hip Arthroplasty.Adv Orthop.2017;2017:8925050. [30] TACK P, VICTOR J, GEMMEL P, et al. 3D-printing techniques in a medical setting: a systematic literature review.Biomed Eng Online. 2016;15(1):115. [31] BAGARIA V, CHAUDHARY K. A paradigm shift in surgical planning and simulation using 3Dgraphy: Experience of first 50 surgeries done using 3D-printed biomodels.Injury.2017;48(11):2501-2508. [32] WANG Q, GOSWAMI K, SHOHAT N, et al. Longer Operative Time Results in a Higher Rate of Subsequent Periprosthetic Joint Infection in Patients Undergoing Primary Joint Arthroplasty.J Arthroplasty.2019; 34(5):947-953. [33] HARRIS WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation.J Bone Joint Surg Am. 1969;51(4):737-755. [34] SHOJI T, YASUNAGA Y, YAMASAKI T, et al. Low femoral antetorsion and total hip arthroplasty: a risk factor.Int Orthop.2015;39(1):7-12. [35] HISATOME T, DOI H. Theoretically optimum position of the prosthesis in total hip arthroplasty to fulfill the severe range of motion criteria due to neck impingement.J Orthop Sci.2011;16(2):229-237. [36] 张江涛,尚延春,吴富源,等.髋关节假体置换中股骨头直径及髋臼前倾角的作用[J].中国组织工程研究,2013,17(30):5427-5433. [37] D'LIMA DD, URQUHART AG, BUEHLER KO,et al. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios.J Bone Joint Surg Am. 2000;82(3):315-321. [38] BARSOUM WK, PATTERSON RW, HIGUERA C, et al.A computer model of the position of the combined component in the prevention of impingement in total hip replacement.J Bone Joint Surg Br.2007; 89(6):839-845. [39] 刘奎玉,赵建宁,钱红波,等.髋臼杯的安放角度对假体稳定性的影响[J].解剖与临床,2013,18(6):524-526. [40] WIDMER KH, ZURFLUH B. Compliant positioning of total hip components for optimal range of motion.J Orthop Res.2004;22(4): 815-821. |
| [1] | Lu Dezhi, Mei Zhao, Li Xianglei, Wang Caiping, Sun Xin, Wang Xiaowen, Wang Jinwu. Digital design and effect evaluation of three-dimensional printing scoliosis orthosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1329-1334. |
| [2] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [3] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [4] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [5] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [6] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [7] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [8] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [9] | Liu Zhengpeng, Wang Yahui, Zhang Yilong, Ming Ying, Sun Zhijie, Sun He. Application of 3D printed interbody fusion cage for cervical spondylosis of spinal cord type: half-year follow-up of recovery of cervical curvature and intervertebral height [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 849-853. |
| [10] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [11] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [12] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [13] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [14] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [15] | Xu Junma, Yu Yuechao, Liu Zhi, Liu Yu, Wang Feitong. Application of 3D-printed coplanar template combined with fixed needle technique in percutaneous accurate biopsy of small pulmonary nodules [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 761-764. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||